What is a Dead Tooth?
A dead tooth, also known as a non-vital tooth, is a tooth where the nerve and blood supply inside the tooth have been damaged or cut off. This often results from severe trauma, extensive decay, or a deep cavity. The pulp, which contains nerves, blood vessels, and connective tissues, dies, causing the tooth to lose its vitality. When a tooth dies, it often darkens, turning gray, brown, or even black. This discoloration is due to the breakdown of red blood cells within the tooth’s structure. The absence of blood flow also means the tooth can become brittle and prone to fracture. If left untreated, a dead tooth can lead to infection, abscesses, and other serious dental problems. The appearance of a dead tooth can also significantly impact a person’s smile and self-esteem, making seeking treatment an important step toward restoring oral health and confidence.
Signs and Symptoms of a Dead Tooth
Recognizing the signs and symptoms of a dead tooth is crucial for early intervention and effective treatment. One of the most noticeable signs is a change in tooth color. The tooth may become darker, appearing gray, brown, or black. This discoloration is often the first indication of a problem. Another common symptom is pain, which can range from mild sensitivity to severe, throbbing discomfort. The pain may come and go or be constant, and it can be triggered by biting, chewing, or exposure to hot or cold temperatures. You might also experience swelling in the gums around the affected tooth or notice a pimple-like bump on the gums, which could indicate an abscess. A foul taste or odor in the mouth can also be a sign of infection. In some cases, there may be no pain at all, especially in the early stages, making regular dental check-ups even more important. If you experience any of these symptoms, it is important to consult a dentist as soon as possible to determine the cause and receive appropriate treatment.
Causes of a Dead Tooth

Several factors can contribute to a tooth becoming non-vital. The most common cause is severe tooth decay. When decay progresses deep into the tooth, it can reach the pulp, infecting it and cutting off the blood supply. Another major cause is trauma to the tooth. A hard blow to the mouth from an accident, sports injury, or other incident can damage the nerves and blood vessels within the tooth, leading to its death. Extensive dental work, such as multiple fillings or crowns, can also increase the risk, especially if the procedures are done close to the pulp. In some cases, the cause of a dead tooth may not be immediately apparent. Other factors, such as repeated dental procedures, can also contribute to pulp damage. Understanding the causes of a dead tooth can help in prevention. For example, wearing a mouthguard during contact sports can protect teeth from trauma. Practicing good oral hygiene, including regular brushing and flossing, can help prevent tooth decay. Early detection and treatment of dental issues are also important to minimize the risk of a tooth becoming non-vital.
Impact of a Dead Tooth on Oral Health
A dead tooth poses several risks to overall oral health if left untreated. The primary concern is the potential for infection. Without a blood supply to fight off bacteria, the dead pulp becomes a breeding ground for infection. This infection can spread to the surrounding tissues, leading to an abscess, a painful collection of pus. An untreated abscess can lead to more serious complications, such as bone loss and the spread of infection to other parts of the body. In addition to infection, a dead tooth can also weaken the structure of the tooth. The lack of blood flow makes the tooth more brittle and prone to fracture. This can lead to further complications, such as the need for extraction. The discoloration caused by a dead tooth can also affect a person’s self-esteem and confidence. The dark appearance can make the smile look unattractive, leading to social anxiety and a reluctance to smile. Therefore, addressing a dead tooth promptly is important not only for oral health but also for overall well-being.
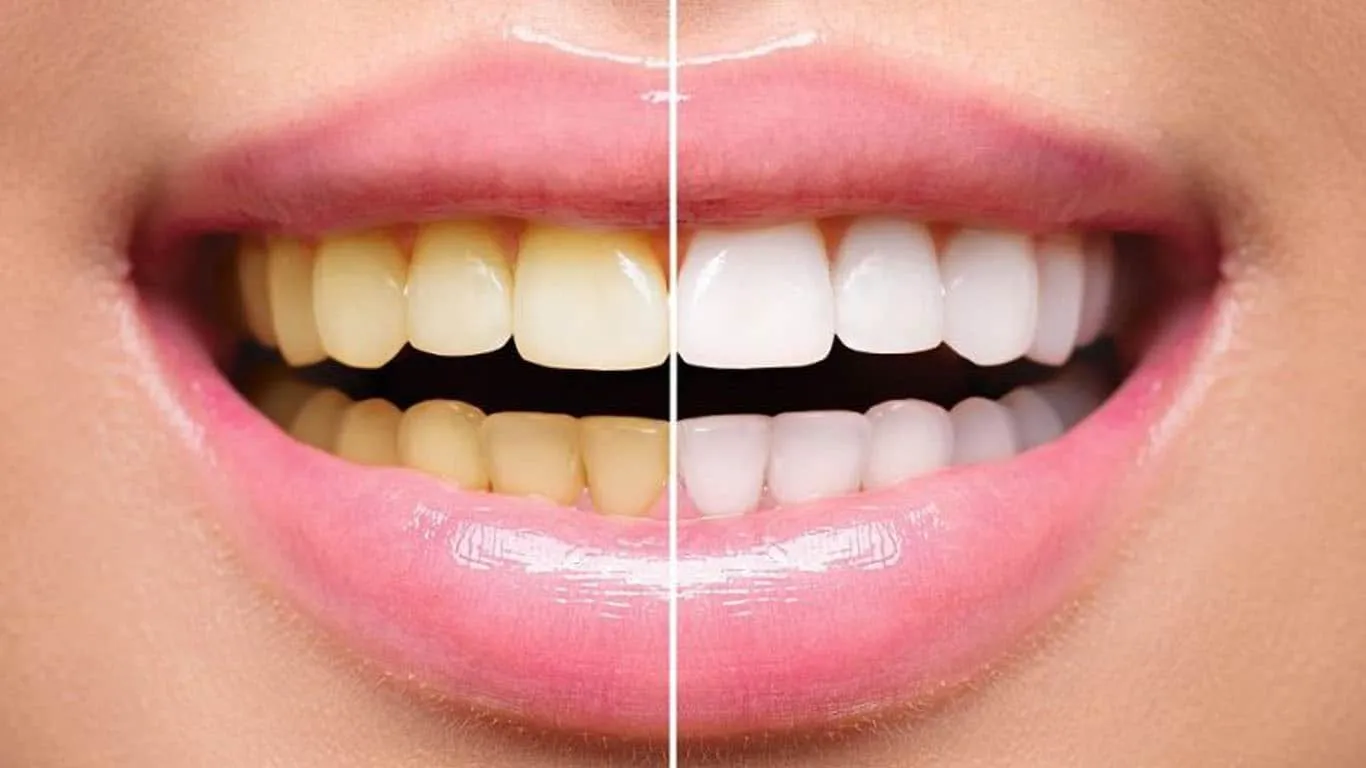
How Dead Tooth Whitening Works
Whitening a dead tooth involves special techniques and procedures aimed at restoring the tooth’s original color. Because the discoloration is caused by internal factors, such as the breakdown of blood cells, traditional teeth whitening methods that work on the surface of the tooth are often ineffective. The primary methods used for whitening a dead tooth include internal bleaching and sometimes external bleaching, depending on the specific condition and the dentist’s assessment. Internal bleaching involves placing a bleaching agent inside the tooth, which is then sealed and left to work for a period of time. External bleaching may be used to address any surface stains or discoloration that remains after internal bleaching. The process is often more complex than standard teeth whitening and may require multiple visits to the dentist. The goal is to lighten the tooth from the inside out, restoring a natural and uniform color that blends with the surrounding teeth. It’s important to note that dead tooth whitening is not always a guarantee, and the success of the treatment can vary depending on the severity of the discoloration and the overall condition of the tooth.
Internal Bleaching

Internal bleaching is the most common and effective method for whitening a dead tooth. The procedure begins with the dentist accessing the pulp chamber of the tooth, usually through the back of the tooth or a small opening in the crown. Any remaining debris and the gutta-percha filling from a previous root canal are removed. A bleaching agent, typically a concentrated hydrogen peroxide solution, is then placed inside the tooth. The dentist seals the tooth with a temporary filling to keep the bleaching agent in place. The patient may need to return to the dentist for several appointments. The bleaching agent is removed and reapplied at each visit until the desired shade is achieved. Once the tooth has reached the desired color, the dentist will permanently seal the tooth. This often involves placing a new filling or a crown to restore the tooth’s strength and appearance. Internal bleaching is a minimally invasive procedure that can significantly improve the appearance of a dead tooth, restoring the patient’s smile and confidence.
External Bleaching
In some cases, external bleaching may be used in conjunction with internal bleaching to further enhance the whitening effect of a dead tooth. External bleaching involves applying a bleaching agent to the outer surface of the tooth. This method is often used to address any surface stains or discoloration that may remain after internal bleaching. The dentist will apply the bleaching agent to the tooth, typically using a custom-fitted tray or a professional-strength whitening gel. The bleaching agent may need to be applied for a specific period, and the procedure may be repeated over several sessions to achieve the desired results. External bleaching is often used to treat a dead tooth that has a minor discoloration. It is a less invasive procedure than internal bleaching and can be performed at home with the dentist’s guidance or in the dental office. While external bleaching may not always be sufficient to whiten a severely discolored dead tooth on its own, it can provide an added boost to the whitening process.
Other Whitening Methods
Besides internal and external bleaching, other methods can improve the appearance of a dead tooth. Dental veneers, thin shells of porcelain or composite resin, can be bonded to the front surface of the tooth to cover the discoloration. Veneers are custom-made to match the shade of the surrounding teeth, providing a natural-looking result. Crowns are another option. They completely cover the tooth, providing both cosmetic and structural benefits. Crowns are especially useful if the dead tooth is weak or damaged. The choice of method depends on the severity of the discoloration and the dentist’s recommendations. In cases where the tooth is severely damaged or cannot be whitened effectively, extraction and replacement with an implant or bridge may be the best option. Each of these treatments has its advantages and disadvantages, and the best approach depends on the individual patient’s needs and the dentist’s evaluation.
Professional Whitening

Professional teeth whitening is a procedure performed in a dentist’s office and is generally more effective than over-the-counter options. The dentist will assess the condition of the teeth and determine the appropriate whitening method. Professional whitening involves the use of higher concentrations of bleaching agents, such as hydrogen peroxide, which can produce dramatic results in a shorter time. The dentist will apply the bleaching agent to the teeth and may use a special light or laser to accelerate the whitening process. The procedure can typically be completed in a single visit, with results visible immediately. Professional whitening offers several advantages, including the use of stronger bleaching agents, which can tackle stubborn stains and discoloration, and the supervision of a dental professional, which ensures the safety and effectiveness of the procedure. In the context of whitening a dead tooth, professional whitening often involves internal bleaching, where the bleaching agent is placed inside the tooth. This targeted approach helps to address the discoloration from within.
Home Whitening Kits
Home whitening kits provide a convenient option for teeth whitening. These kits typically contain custom-fitted trays and a bleaching agent, which is typically a lower concentration of hydrogen peroxide. The dentist will often provide instructions on using the kit. The patient fills the tray with the bleaching gel and wears it for a specific period each day, as recommended by the dentist. Home whitening kits are less effective than professional whitening and may take longer to produce visible results. They can be a good option for maintaining the results of professional whitening or for addressing mild discoloration. It’s important to follow the dentist’s instructions carefully. Overuse of the bleaching agent can cause sensitivity and other side effects. In the case of a dead tooth, home whitening kits are generally not effective for internal discoloration. They may be used to address minor surface stains after professional treatment. Before using any home whitening product, it is best to consult with a dentist to ensure it is safe and appropriate for your specific needs.
Maintenance and Aftercare Tips
Maintaining the results of dead tooth whitening involves several steps. First, practice good oral hygiene habits. Brush your teeth twice a day with fluoride toothpaste and floss daily to remove plaque and food particles. Avoid foods and beverages that can stain teeth, such as coffee, tea, red wine, and dark-colored berries. If you consume these items, rinse your mouth with water immediately afterward. Use a straw when drinking staining beverages to minimize contact with the teeth. Regular dental check-ups and cleanings are also essential. The dentist can monitor the color of the teeth and provide professional cleaning to remove surface stains. Consider using a whitening toothpaste or mouthwash to help maintain the brightness of your smile. If you smoke, consider quitting, as smoking can stain teeth and reduce the effectiveness of whitening treatments. By following these maintenance and aftercare tips, you can help ensure long-lasting results from dead tooth whitening and maintain a healthy, bright smile.
Preventing Dead Teeth
Preventing a tooth from becoming non-vital involves protecting the teeth from the factors that cause pulp damage. Good oral hygiene is the first line of defense. Brushing and flossing regularly help prevent tooth decay, one of the leading causes of dead teeth. Regular dental check-ups and cleanings are crucial for early detection and treatment of dental issues. Visiting the dentist twice a year allows for the identification of cavities and other problems before they progress and damage the pulp. Protecting teeth from injury is also important. Wear a mouthguard during contact sports or any activity that poses a risk of trauma to the mouth. If you grind your teeth, consider using a nightguard to protect them from excessive wear and tear. Addressing dental problems promptly is crucial. Seek immediate treatment for any tooth pain, sensitivity, or other symptoms to prevent the problem from worsening and potentially affecting the pulp. Following these preventive measures, you can significantly reduce the risk of a tooth becoming non-vital and maintain a healthy, bright smile.
Regular Dental Check-ups
Regular dental check-ups are a cornerstone of maintaining oral health. They involve a comprehensive examination of the teeth, gums, and surrounding tissues. The dentist will check for signs of decay, gum disease, and other dental problems. Professional cleaning removes plaque and tartar, which can cause cavities and gum disease. X-rays may be taken to detect problems that are not visible to the naked eye, such as cavities between teeth or infections in the jawbone. During a check-up, the dentist may also provide advice on oral hygiene practices, such as proper brushing and flossing techniques. Early detection and treatment of dental problems through regular check-ups can prevent many serious issues. They help maintain healthy teeth and gums, which are essential for overall health and well-being. Regular check-ups can identify potential problems early on, allowing for prompt intervention and reducing the need for more extensive treatments. Scheduling check-ups every six months is generally recommended, but the frequency may vary depending on individual needs and risk factors.
Protecting Teeth from Injury
Protecting teeth from injury is crucial for preventing trauma-related issues, including a dead tooth. Wearing a mouthguard during sports and recreational activities is essential. Mouthguards cushion the teeth and protect them from direct blows. Custom-fitted mouthguards, made by a dentist, provide the best protection, as they fit the mouth perfectly. For individuals who grind their teeth, using a nightguard can protect the teeth from excessive wear and tear. Nightguards also help to distribute the forces of grinding, reducing the risk of tooth damage. Avoiding chewing on hard objects, such as ice, pencils, or hard candies, can also prevent tooth fractures and other injuries. Being mindful of your surroundings and taking precautions to avoid falls or accidents can also minimize the risk of trauma to the teeth. If a tooth is injured, seeking immediate dental attention is essential. Prompt treatment can increase the chances of saving the tooth and preventing further complications. Taking proactive steps to protect your teeth can help preserve your smile and avoid the need for more complex dental procedures.
The Cost of Dead Tooth Whitening

The cost of whitening a dead tooth can vary significantly depending on the specific treatment required and the dentist’s fees. Internal bleaching is typically the most common method, and the cost will depend on the number of visits needed and the complexity of the procedure. External bleaching, if used, will add to the overall cost. Other treatments, such as veneers or crowns, will cost more than whitening. The geographical location and the dentist’s experience also influence the cost. Consulting with your dentist is the best way to get an accurate estimate of the total cost. Many dental insurance plans may cover a portion of the costs for certain treatments, such as endodontic procedures or crowns. Discuss your insurance coverage with your dentist or insurance provider. Explore financing options to make the treatment more affordable. Many dental offices offer payment plans or work with third-party financing companies to help patients manage the cost of dental procedures. It is important to discuss the cost and all available options with your dentist to make an informed decision.
Conclusion
Whitening a dead tooth can restore both the aesthetic and functional aspects of a damaged tooth. While a dead tooth can be a cause for concern, advancements in dental treatments provide effective solutions to address this issue. Internal and external bleaching offer ways to restore the tooth’s original color. Other methods, like veneers and crowns, provide additional options for restoring the tooth’s appearance and structural integrity. Prevention through good oral hygiene, regular dental check-ups, and protecting your teeth from injury remains crucial. Understanding the causes, symptoms, and treatment options for a dead tooth can empower individuals to take proactive steps towards maintaining a healthy, bright smile. Consulting with a dentist is the most important step in determining the best course of treatment for your specific needs, ensuring the long-term health and beauty of your teeth.
